What is PRP?
Platelet-Rich Plasma (PRP) is made of patient's own blood and is currently used in the sports and regenerative medicine for wound and injury healing and tissue regeneration; in the treatment of the thinning hair; and in the face and skin rejuvenation treatments.
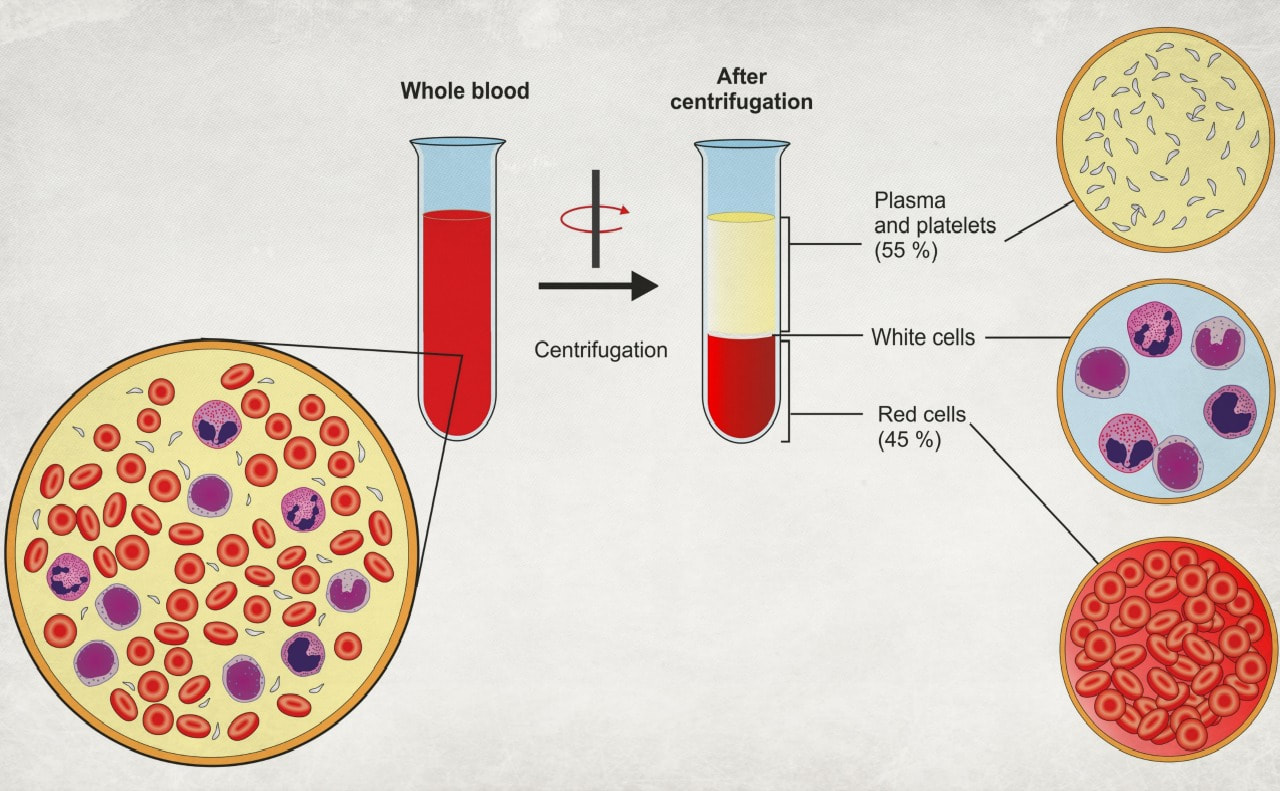
PRP treatments are relatively non-invasive and regarded as safe. The patient's own blood is drawn from the vein. Then a vial with the blood is spun in a centrifuge to separate red blood cells, white blood cells, and platelet poor plasma from the PRP - platelet-rich-plasma. The former are all discarded, and the remaining golden-color PRP liquid is activated with thrombin and calcium and is used in the treatment.
Concentration of the platelets in PRP is 3-7 times higher than in the whole blood. 10 ml of blood produce between 1.5 and 4 ml of PRP.
The better quality the blood, the more effective the treatment will be. For this reason it is recommended to eat healthy diet prior to the treatment.
Platelet-Rich Plasma (PRP) is made of patient's own blood and is currently used in the sports and regenerative medicine for wound and injury healing and tissue regeneration; in the treatment of the thinning hair; and in the face and skin rejuvenation treatments.
PRP treatments are relatively non-invasive and regarded as safe. The patient's own blood is drawn from the vein. Then a vial with the blood is spun in a centrifuge to separate red blood cells, white blood cells, and platelet poor plasma from the PRP - platelet-rich-plasma. The former are all discarded, and the remaining golden-color PRP liquid is activated with thrombin and calcium and is used in the treatment.
Concentration of the platelets in PRP is 3-7 times higher than in the whole blood. 10 ml of blood produce between 1.5 and 4 ml of PRP.
The better quality the blood, the more effective the treatment will be. For this reason it is recommended to eat healthy diet prior to the treatment.
|
Is PRP effective for skin and face rejuvenation? Why and how does it work?
PRP is used for the skin rejuvenation on the face, hands, chest (décolleté). Clinical research and studies published in medical journals show that -
The science and theory behind the PRP treatments is that when concentrated in the PRP platelets are activated, they produce and release various bioactive proteins and peptides called growth factors (Alsousou, 2009; Civinini, 2010). The released growth factors exert effect of cell growth, stimulate stem cells and fibroblasts, which in turn, increase production of collagen (Abuaf, 2016) and creation of the new healthy, younger looking tissue (Fukaya, 2014; Kakudo, 2008; Khatu, 2014; Kim, 2011). The complete and precise mechanisms of how PRP works have not been fully explained and proven. You can read more about growth factors at the end of the publication. |
The optimized method of PRP preparation that aims at achieving the optimal concentration of platelets is covered in this study (Araki, 2012).
How is PRP treatment for facial rejuvenation performed?
PRP can be "administered" to the treated area in two ways:
- Applied on the face immediately after a micro-needling session that created thousands of microscopic skin punctures. PRP essentially soaks into the dermis, and possibly deeper, through the needle created holes in the epidermis;
- Injected with a needle. When PRP is injected with a needle it is sometimes referred to as a Vampire Facelift.
The cost of a single PRP/PRFM session is relatively high and varies between $500 - $1000 per treated area.
Both the con and the pro of the PRP treatments is that the result is not immediate; it is gradual and builds over time as the skin rejuvenates itself.
PRP can be "administered" to the treated area in two ways:
- Applied on the face immediately after a micro-needling session that created thousands of microscopic skin punctures. PRP essentially soaks into the dermis, and possibly deeper, through the needle created holes in the epidermis;
- Injected with a needle. When PRP is injected with a needle it is sometimes referred to as a Vampire Facelift.
The cost of a single PRP/PRFM session is relatively high and varies between $500 - $1000 per treated area.
Both the con and the pro of the PRP treatments is that the result is not immediate; it is gradual and builds over time as the skin rejuvenates itself.
PRFM
PRFM (Platelet Rich Fibrin Matrix) is a variation of PRP. It involves an additional processing step with the addition of calcium chloride. Thus, a fibrin matrix is created that protects the platelets and supports a sustained release of the grown factors at the injection site for several days after the treatment.
PRFM (Platelet Rich Fibrin Matrix) is a variation of PRP. It involves an additional processing step with the addition of calcium chloride. Thus, a fibrin matrix is created that protects the platelets and supports a sustained release of the grown factors at the injection site for several days after the treatment.
Growth Factors in PRP
Platelets are a part of our bodies' mechanism of healing itself. In response to an injury, blood platelets release growth factors that initiate, support, and promote healing. The growth factors are bioactive peptides and proteins, which are supposedly the reason behind the healing and rejuvenating properties of PRP. The table below lists the growth factor released by platelets and their functions.
Platelets are a part of our bodies' mechanism of healing itself. In response to an injury, blood platelets release growth factors that initiate, support, and promote healing. The growth factors are bioactive peptides and proteins, which are supposedly the reason behind the healing and rejuvenating properties of PRP. The table below lists the growth factor released by platelets and their functions.
FGF |
Fibroblast growth factors |
Participate in tissue repair, cell growth, collagen production. There are 22 of them |
TGF-b |
Transforming growth factor Beta |
Initiates growth and neogenesis of epithelial cells and vascular endothelial cells; promotes wound healing |
PDGF |
Platelet derived growth factor |
Supports collagen production, cell growth, new generation and repair of blood vessels |
EGF |
Epidermal/epithelial growth factor |
Promotes epithelial cell growth, wound healing, angiogenesis |
VEGF |
Vascular endothelial growth factor |
Promotes wound healing and angiogenesis |
KGF |
Keratinocyte growth factor |
Promotes keratinocyte growth |
IGF |
Insulin-like growth factor |
Regulates cell growth |
IL-1 |
Interleukin-1 |
Stimulates proliferation of dermal fibroblasts; activates production of collagen |
(Yun, 2010; Alsousou, 2009; Pomytkin, 2015)
Treatment Specific References and Literature
Abuaf OK, Yildiz H, Baloglu H, Bilgili ME, Simsek HA, Dogan B. Histologic Evidence of New Collagen Formulation Using Platelet Rich Plasma in Skin Rejuvenation: A Prospective Controlled Clinical Study. Annals of Dermatology. 2016;28(6):718-724. doi:10.5021/ad.2016.28.6.718.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5125953/
Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br. 2009;91(08):987–996.
http://bjj.boneandjoint.org.uk/content/91-B/8/987.long
Araki J, Jona M, Eto H, et al. Optimized preparation method of platelet-concentrated plasma and noncoagulating platelet-derived factor concentrates: maximization of platelet concentration and removal of fibrinogen. Tissue Eng Part C Methods. 2011;18(3):176-85.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285602/
Cabrera-Ramírez, J.O., Puebla-Mora, A.G., González-Ojeda, A., García-Martínez, D., Cortés-Lares, J.A., Márquez-Valdéz, A.R., Contreras-Hernández, G.I., Bracamontes-Blanco, J., Saucedo-Ortíz, J.A., Fuentes-Orozco, C. Platelet-Rich Plasma for the Treatment of Photodamage of the Skin of the Hands
Actas Dermosifiliogr 2017;108:746-51 - Vol. 108 Num.8 DOI: 10.1016/j.adengl.2017.07.002
https://www.ncbi.nlm.nih.gov/pubmed/28625328
Civinini R, Macera A, Redl B, Innocenti M. Blood-Derived Growth Factors. Clinical Cases in Mineral and Bone Metabolism. 2010;7(3):194. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3213779/
Dhurat R, Sukesh M. Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author’s Perspective. Journal of Cutaneous and Aesthetic Surgery. 2014;7(4):189-197. doi:10.4103/0974-2077.150734.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4338460/
Elnehrawy, N. Y., Ibrahim, Z. A., Eltoukhy, A. M. and Nagy, H. M. (2017), Assessment of the efficacy and safety of single platelet-rich plasma injection on different types and grades of facial wrinkles. J Cosmet Dermatol, 16: 103–111. doi:10.1111/jocd.12258
https://www.ncbi.nlm.nih.gov/pubmed/27474688
Fukaya M, Ito A. A New Economic Method for Preparing Platelet-rich Plasma. Plastic and Reconstructive Surgery Global Open. 2014;2(6):e162. doi:10.1097/GOX.0000000000000109.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4174234/
Gentile P, Garcovich S, Bielli A, Scioli MG, Orlandi A, Cervelli V. The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomized Placebo-Controlled Trial. Stem Cells Translational Medicine. 2015;4(11):1317-1323. doi:10.5966/sctm.2015-0107.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622412/
Kakudo N, Minakata T, Mitsui T, Kushida S, Notodihardjo FZ, Kusumoto K. Proliferation-promoting effect of platelet-rich plasma on human adipose-derived stem cells and human dermal fibroblasts. Plast Reconstr Surg. 2008;122(5):1352-1360.
https://www.ncbi.nlm.nih.gov/pubmed/18971718
Khatu SS, More YE, Gokhale NR, Chavhan DC, Bendsure N. Platelet-Rich Plasma in Androgenic Alopecia: Myth or an Effective Tool. Journal of Cutaneous and Aesthetic Surgery. 2014;7(2):107-110. doi:10.4103/0974-2077.138352.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4134641/
Kim DH, Je YJ, Kim CD, et al. Can Platelet-rich Plasma Be Used for Skin Rejuvenation? Evaluation of Effects of Platelet-rich Plasma on Human Dermal Fibroblast. Annals of Dermatology. 2011;23(4):424-431. doi:10.5021/ad.2011.23.4.424.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229934/
Lee JW, Kwon OH, Kim TK, et al. Platelet-Rich Plasma: Quantitative Assessment of Growth Factor Levels and Comparative Analysis of Activated and Inactivated Groups. Archives of Plastic Surgery. 2013;40(5):530-535. doi:10.5999/aps.2013.40.5.530.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3785585/
Pomytkin I, Schoch P, Skin rejuvenating effects of interleukin-1 alpha. Aesthetics. 2015; Feb.
https://aestheticsjournal.com/feature/skin-rejuvenating-effects-of-interleukin-1-alpha
Sclafani AP, McCormick SA. Induction of Dermal Collagenesis, Angiogenesis, and Adipogenesis in Human Skin by Injection of Platelet-Rich Fibrin Matrix. Arch Facial Plast Surg. 2012;14(2):132–136. doi:10.1001/archfacial.2011.784
https://jamanetwork.com/journals/jamafacialplasticsurgery/fullarticle/1150976
Ulusal, B. G. (2017), Platelet-rich plasma and hyaluronic acid – an efficient biostimulation method for face rejuvenation. J Cosmet Dermatol, 16: 112–119. doi:10.1111/jocd.12271
https://www.ncbi.nlm.nih.gov/pubmed/27595866
Yuksel EP, Sahin G, Aydin F, Senturk N, Turanli AY. Evaluation of effects of platelet-rich plasma on human facial skin. J Cosmet Laser Ther. 2014;16:206–208.
http://www.tandfonline.com/doi/abs/10.3109/14764172.2014.949274
Yun Y-R, Won JE, Jeon E, et al. Fibroblast Growth Factors: Biology, Function, and Application for Tissue Regeneration. Journal of Tissue Engineering. 2010;2010:218142. doi:10.4061/2010/218142.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3042641/
Abuaf OK, Yildiz H, Baloglu H, Bilgili ME, Simsek HA, Dogan B. Histologic Evidence of New Collagen Formulation Using Platelet Rich Plasma in Skin Rejuvenation: A Prospective Controlled Clinical Study. Annals of Dermatology. 2016;28(6):718-724. doi:10.5021/ad.2016.28.6.718.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5125953/
Alsousou J, Thompson M, Hulley P, Noble A, Willett K. The biology of platelet-rich plasma and its application in trauma and orthopaedic surgery: a review of the literature. J Bone Joint Surg Br. 2009;91(08):987–996.
http://bjj.boneandjoint.org.uk/content/91-B/8/987.long
Araki J, Jona M, Eto H, et al. Optimized preparation method of platelet-concentrated plasma and noncoagulating platelet-derived factor concentrates: maximization of platelet concentration and removal of fibrinogen. Tissue Eng Part C Methods. 2011;18(3):176-85.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285602/
Cabrera-Ramírez, J.O., Puebla-Mora, A.G., González-Ojeda, A., García-Martínez, D., Cortés-Lares, J.A., Márquez-Valdéz, A.R., Contreras-Hernández, G.I., Bracamontes-Blanco, J., Saucedo-Ortíz, J.A., Fuentes-Orozco, C. Platelet-Rich Plasma for the Treatment of Photodamage of the Skin of the Hands
Actas Dermosifiliogr 2017;108:746-51 - Vol. 108 Num.8 DOI: 10.1016/j.adengl.2017.07.002
https://www.ncbi.nlm.nih.gov/pubmed/28625328
Civinini R, Macera A, Redl B, Innocenti M. Blood-Derived Growth Factors. Clinical Cases in Mineral and Bone Metabolism. 2010;7(3):194. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3213779/
Dhurat R, Sukesh M. Principles and Methods of Preparation of Platelet-Rich Plasma: A Review and Author’s Perspective. Journal of Cutaneous and Aesthetic Surgery. 2014;7(4):189-197. doi:10.4103/0974-2077.150734.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4338460/
Elnehrawy, N. Y., Ibrahim, Z. A., Eltoukhy, A. M. and Nagy, H. M. (2017), Assessment of the efficacy and safety of single platelet-rich plasma injection on different types and grades of facial wrinkles. J Cosmet Dermatol, 16: 103–111. doi:10.1111/jocd.12258
https://www.ncbi.nlm.nih.gov/pubmed/27474688
Fukaya M, Ito A. A New Economic Method for Preparing Platelet-rich Plasma. Plastic and Reconstructive Surgery Global Open. 2014;2(6):e162. doi:10.1097/GOX.0000000000000109.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4174234/
Gentile P, Garcovich S, Bielli A, Scioli MG, Orlandi A, Cervelli V. The Effect of Platelet-Rich Plasma in Hair Regrowth: A Randomized Placebo-Controlled Trial. Stem Cells Translational Medicine. 2015;4(11):1317-1323. doi:10.5966/sctm.2015-0107.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4622412/
Kakudo N, Minakata T, Mitsui T, Kushida S, Notodihardjo FZ, Kusumoto K. Proliferation-promoting effect of platelet-rich plasma on human adipose-derived stem cells and human dermal fibroblasts. Plast Reconstr Surg. 2008;122(5):1352-1360.
https://www.ncbi.nlm.nih.gov/pubmed/18971718
Khatu SS, More YE, Gokhale NR, Chavhan DC, Bendsure N. Platelet-Rich Plasma in Androgenic Alopecia: Myth or an Effective Tool. Journal of Cutaneous and Aesthetic Surgery. 2014;7(2):107-110. doi:10.4103/0974-2077.138352.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4134641/
Kim DH, Je YJ, Kim CD, et al. Can Platelet-rich Plasma Be Used for Skin Rejuvenation? Evaluation of Effects of Platelet-rich Plasma on Human Dermal Fibroblast. Annals of Dermatology. 2011;23(4):424-431. doi:10.5021/ad.2011.23.4.424.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3229934/
Lee JW, Kwon OH, Kim TK, et al. Platelet-Rich Plasma: Quantitative Assessment of Growth Factor Levels and Comparative Analysis of Activated and Inactivated Groups. Archives of Plastic Surgery. 2013;40(5):530-535. doi:10.5999/aps.2013.40.5.530.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3785585/
Pomytkin I, Schoch P, Skin rejuvenating effects of interleukin-1 alpha. Aesthetics. 2015; Feb.
https://aestheticsjournal.com/feature/skin-rejuvenating-effects-of-interleukin-1-alpha
Sclafani AP, McCormick SA. Induction of Dermal Collagenesis, Angiogenesis, and Adipogenesis in Human Skin by Injection of Platelet-Rich Fibrin Matrix. Arch Facial Plast Surg. 2012;14(2):132–136. doi:10.1001/archfacial.2011.784
https://jamanetwork.com/journals/jamafacialplasticsurgery/fullarticle/1150976
Ulusal, B. G. (2017), Platelet-rich plasma and hyaluronic acid – an efficient biostimulation method for face rejuvenation. J Cosmet Dermatol, 16: 112–119. doi:10.1111/jocd.12271
https://www.ncbi.nlm.nih.gov/pubmed/27595866
Yuksel EP, Sahin G, Aydin F, Senturk N, Turanli AY. Evaluation of effects of platelet-rich plasma on human facial skin. J Cosmet Laser Ther. 2014;16:206–208.
http://www.tandfonline.com/doi/abs/10.3109/14764172.2014.949274
Yun Y-R, Won JE, Jeon E, et al. Fibroblast Growth Factors: Biology, Function, and Application for Tissue Regeneration. Journal of Tissue Engineering. 2010;2010:218142. doi:10.4061/2010/218142.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3042641/